What is in this leaflet
This leaflet answers some common questions about JURNISTA prolonged-release tablets. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking JURNISTA against the benefits this medicine is expected to have for you.
If you have any concerns about taking JURNISTA, ask your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What JURNISTA is taken for
JURNISTA is taken to relieve moderate to severe pain, which requires strong painkillers.
JURNISTA is only for patients with chronic, around the clock pain that is moderate to severe and expected to be long lasting. JURNISTA is not used to treat pain on an as-needed basis.
JURNISTA should not be the first medicine prescribed for your pain.
JURNISTA prolonged-release tablets contain a medicine called hydromorphone hydrochloride. This strong pain reliever belongs to a group of medicines known as opioid analgesics. Hydromorphone hydrochloride relieves pain by blocking the nerves that recognise pain messages from the body.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
Before you take JURNISTA
Warning
Addiction
You can become addicted to JURNISTA even if you take it exactly as prescribed. JURNISTA may become habit forming causing mental and physical dependence. If abused it may become less able to reduce pain.
Dependence
As with all other opioid containing products, your body may become used to you taking JURNISTA. Taking it may result in physical dependence. Physical dependence means that you may experience withdrawal symptoms if you stop taking JURNISTA suddenly, so it is important to take it exactly as directed by your doctor.
Tolerance
Tolerance to JURNISTA may develop, which means that the effect of the medicine may decrease. If this happens, more may be needed to maintain the same effect.
Withdrawal
Continue taking your medicine for as long as your doctor tells you. If you stop having this medicine suddenly, your pain may worsen and you may experience some or all of the following withdrawal symptoms:
- nervousness, restlessness, agitation, trouble sleeping or anxiety
- body aches, weakness or stomach cramps
- loss of appetite, nausea, vomiting or diarrhoea
- increased heart rate, breathing rate or pupil size
- watery eyes, runny nose, chills or yawning
- increased sweating.
JURNISTA given to the mother during labour can cause breathing problems and signs of withdrawal in the newborn.
Increased sensitivity to pain
Rarely, increasing the dose of this medicine can make you more sensitive to pain. If this happens, you need to speak to your doctor about your treatment.
When you must not take it
Do not take JURNISTA if you:
- have an allergy to hydromorphone hydrochloride or any of the ingredients. See Product Description at the end of this leaflet for a list of ingredients.
- have been diagnosed with serious narrowing of the stomach and/or intestine (bowel)
- have pain resulting from very recent surgery or sudden pain which is long lasting
- have had surgery which may have left you with 'blind loop' in your intestine
- have seriously impaired liver function
- have serious breathing difficulties, with slow or shallow breathing
- have severe acute asthma
- get sudden severe abdominal pain and the cause hasn't been diagnosed
- are taking a type of antidepressants called Monoamine Oxidase (MAO) inhibitors, or have taken them within the last 14 days
- are taking other morphine-related painkillers (buprenorphine, nalbuphine or pentazocine).
- have not used any opioid analgesics in the past. This is because you may be more likely to experience some of the side effects
Do not take JURNISTA if the packaging is torn or shows signs of tampering.
Do not take JURNISTA beyond the expiry date (month and year) printed on the pack. If you take this medicine after the expiry date has passed, it may not work as well.
Do not give JURNISTA to babies or children, women during pregnancy, labour, delivery, breastfeeding or patients who are in a coma. JURNISTA should not be used during childbirth as the medicine can slow the breathing of the newborn child. Prolonged use of JURNISTA during pregnancy can cause withdrawal symptoms in your newborn baby that could be life-threatening if not recognised and treated.
Before you start to take it
You must tell your doctor if you:
- are pregnant or planning to become pregnant
- are breastfeeding or wish to breastfeed
- have not used any opioid analgesics in the past
- have or have ever had any problems with your liver or kidney
- have or have ever had any problems with your lungs or difficulty in breathing
- have a history of sleep apnoea or if anyone notices you stop breathing from time to time whilst sleeping
- have or have ever had heart disorders
- have or ever had headaches or head injuries
- have or ever had chronic constipation or any disease of your intestine including obstruction or inflammatory bowel disease
- have or ever had inflammation of the pancreas (pancreatitis) or disease of the bile duct
- you or your family have a history of substance dependence or abuse of drugs, alcohol or any opioid painkillers or mental illness
- had a severe reaction, such as confusion and shaking, to stopping alcohol (sometimes called delirium tremens)
- have or ever had symptoms of CNS depression such as severe drowsiness, low body temperature and sometimes coma
- have or ever had fits or seizures
- have an under-active thyroid (hypothyroidism) or problems with your adrenal gland
- have an enlarged prostate
- have difficulty in passing urine
- have a major mental disorder following an infection (toxic psychosis)
- have abnormal curvature of the spine (kyphoscoliosis)
- are planning to have a surgery
- are sensitive to sulfite
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking or are given JURNISTA.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including medicines you can buy without a prescription from a pharmacy, supermarket or health food shop.
In particular, tell your doctor or pharmacist if you are taking any of the following:
- medicines that slow down your central nervous system, (for example:
− medicines that makes you sleepy, reduce anxiety such as sedatives, hypnotics, sleeping tablets, tranquillisers (benzodiazepines),
− other opioid medicines
− medicines used for surgery (anaesthetics) and, muscle relaxants ,
− antihistamines or allergy medicine that makes you drowsy ,
− gabapentinoid medicines used to treat epilepsy or nerve pain such as gabapentin and pregabalin
− alcohol, cannabis or some illegal drugs.
Taking these medicines with JURNISTA may make you even more drowsy, slow down your ability to react, have decrease awareness, breathing difficulties with slow or shallow breathing, coma and death. A change in dose by your doctor may be required if JURNISTA is used with these medicines.
- medicines used as antidepressants. In particular, antidepressants belonging to a group called monoamine oxidase inhibitors (MAOIs), such asmoclobemide, phenelzine sulfate and tranylcypromine sulfate. JURNISTA should not be used together with MAOIs as this may cause severe serotonin syndrome which is a potentially life-threatening condition. Signs and symptoms can include confusion, restlessness, fever, heavy sweating, fast or irregular heart rate, diarrhoea, uncoordinated movement of limbs or eyes, uncontrollable jerking of muscles, seizures and unconsciousness. Do not use JURNISTA if you have taken an MAOI in the last 14 days.
JURNISTA can increase the effect of drugs that are sedating or slow down your ability to react. A change in dose may be required if JURNISTA is taken with these medicines.
Your doctor or pharmacist can tell you what to do if you are taking any of these medicines.
Effect on driving and operating machinery
JURNISTA can make you drowsy.
Do not drive, operate machinery or do hazardous work until you are sure you are not affected.
Take special care if your dose or type of medication is changed.
Effect of alcohol
You must not drink alcohol while taking JURNISTA since their combined effect may cause severe drowsiness, decreased awareness, breathing problems, coma and death.
Warning: If your doctor has told you that you have intolerance to some sugars, including lactose, contact your doctor before taking JURNISTA.
Taking JURNISTA
How to take the tablet
Adults
JURNISTA is available in five different strengths. Your doctor will decide which strength is suitable to control your pain.
The usual starting dose of JURNISTA is 8mg taken at the same time each day. However, your doctor may prescribe a different dose of JURNISTA to start with if you are changing from a different morphine-related painkiller.
The lowest effective dose should be used for the shortest period of time.
JURNISTA should be swallowed whole, with a glass of water.
JURNISTA may be taken with or without food.
DO NOT crush or chew the tablets. If you do, there is a danger you could overdose, because the medicine will be released into your body too quickly. JURNISTA is only designed to work properly if swallowed whole. The tablets may release all their contents at once if broken, chewed, crushed or dissolved, which can be dangerous and cause serious problems, such as an overdose which may be fatal. Unless stated otherwise, they should be swallowed whole.
Do not take JURNISTA more than once every 24 hours. If you have insufficient pain relief from JURNISTA you should contact your doctor for advice. Taking another JURNISTA tablet some time after a first tablet on the same day could result in too much medicine being released into your body.
Ask your doctor or pharmacist for help if you do not understand the instructions provided with this medicine.
Children
JURNISTA should not be given to children and adolescents under 18 years of age.
If you forget to take it
If you forget to take a tablet, take the next dose immediately and start a new 24-hour regimen. If you are not sure what to do, check with your doctor or pharmacist. DO NOT take extra tablets or double dose to make up for the forgotten tablets.
If you have trouble remembering when to take the tablet, ask your pharmacist for some hints.
If you take too much (overdose)
If you or someone else receive too much (overdose), and experience one or more of the symptoms below, call triple zero (000) for an ambulance.
Keep the person awake by talking to them or gently shaking them every now and then. You should follow the above steps even if someone other than you have accidentally used JURNISTA that was prescribed for you. If someone takes an overdose they may experience one or more of the following symptoms:
- Slow, unusual or difficult breathing
- Drowsiness, dizziness or unconsciousness
- Slow or weak heartbeat
- Nausea or vomiting
- Convulsions or fits
If you think you or someone else may have used too much JURNISTA, you should immediately:
- phone the Poisons Information Centre (by calling 13 11 26), or
- contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
When seeking medical attention, take this leaflet and remaining medicine with you to show the doctor. Also tell them about any other medicines or alcohol which have been taken.
INFORMATION FOR THE DOCTOR
In case of overdose: administer an opioid antagonist and transfer patient to hospital.
Please refer to full Product Information for details on appropriate management of overdose.
While you are taking JURNISTA
Things you must do
- Always follow your doctor's instructions carefully.
- Tell your doctor if you become pregnant while taking JURNISTA.
- If you are about to start taking a new medicine, tell your doctor and pharmacist that you are taking JURNISTA.
- If your pain continues or returns, see your doctor. You may need additional medicines to control the pain or a change in the strength of the JURNISTA tablet.
- If there is a change in the pain you are feeling e.g if
- You feel your pain is no longer relieved by the tablets
- you feel an increase in pain
- there is a change in how you feel the pain (for example, you feel pain in another part of your body)
- you feel pain when something touches your body that you wouldn’t expect to hurt you.
Do not change the dose yourself. Your doctor may decide to change your dose or treatment.
DO NOT be alarmed if you notice what appears to be the JURNISTA tablet in your stool; this is simply the non-dissolvable shell of the tablet.
Things you must not do
- DO NOT use JURNISTA to treat any other complaint unless your doctor says so.
- DO NOT give the tablets to anyone else, even if their symptoms seem similar to yours.
- DO NOT stop taking JURNISTA unless your doctor advises you to do so.
If you have been taking JURNISTA for a long period of time but stop taking it suddenly without your doctor's advice, you may experience withdrawal symptoms such as:
- anxiety or irritability
- vomiting or feeling sick
- diarrhoea or stomach pain
- the pupils of your eyes increasing in size
- blushing or sweating
- crying for no reason
- pains in your joints
Seek your doctor's advice if you experience any of these symptoms.
Do not crush and intravenously inject JURNISTA. Animal studies have shown that some of the non-active components of JURNISTA can cause serious damage to organs such as the heart, kidneys, and blood cells and even death, when injected intravenously. When taken by mouth as instructed by your doctor these non-active components of JURNISTA are not absorbed into the body and are well tolerated.
Side effects
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some side effects. Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you experience any of the following:
- nausea, vomiting, cramps, diarrhoea, fever, stomach pain or discomfort, constipation, dry mouth, indigestion, difficulty in swallowing, excessive gas in the stomach or bowel, passage of stools containing blood, piles, abnormal faeces, belching, torn rectum, inflammation of the small intestine, bowel obstruction, painful defecation
- loss of appetite, weight decrease, dehydration, fluid retention, increased appetite, high uric acid levels in the blood, which may cause gout
- nervousness, confusion, hallucinations, euphoria, depression, trouble sleeping, anxiety, abnormal dreams, restlessness, altered mood, decreased sexual drive, panic attack, listless, paranoia, aggression, crying, erectile dysfunction
- sleep apnoea (stopping breathing from time to time whilst sleeping)
- trouble in urinating, pain when passing urine, urinary hesitation, frequent day time urination
- sleepiness, headache, dizziness, increased or decreased feeling, pins and needles, shaking, memory impairment, disturbance in attention, taste disorder, speech disorder, balance disorder, abnormal coordination, uncontrollable twitching, cognitive disorder, convulsion, unusually increased reflexes, buzzing or whistling in the ears
- blurred vision, double vision, dry eyes, contraction of the pupil
- itching, excessive sweating, rash, redness of the skin, skin burning sensation, sneezing
- muscle spasms, back pain, joint pain, pain in extremity, aching muscles
- weakness, pain, chills, drug withdrawal symptoms, feeling unwell or abnormal, difficulty in walking, influenza-like illness.
Tell your doctor immediately if you experience any of the following, as you may need urgent medical care:
- fainting, decreased level of consciousness, cognitive disorder
- fast or irregular heart rate, extra heart beats
- flushing, high or low blood pressure
- shortness or difficulty in breathing, lack of oxygen, respiratory depression, fast breathing
- swelling of the face, lips, mouth, tongue or throat, fever or high temperature, chest discomfort
After taking JURNISTA
Storage
Store JURNISTA securely, where other people cannot access it. It may harm people who may take this medicine by accident, or intentionally when it has not been prescribed for them.
Keep JURNISTA tablets in the blister pack and box until it is time to take them.
Keep the tablets in a cool dry place where temperature is below 25°C.
Keep your medicines where children cannot reach them. A locked cupboard at least one-and-a-half metres (1.5 m) above the ground is a good place to store medicines.
Do not store JURNISTA tablets or any other medicine, in the bathroom or near a sink. Do not leave medicines in the car or on window sills. Heat and dampness can destroy some medicines.
Disposal
If the medicine is damaged, you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
Product description
What it looks like
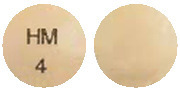
- JURNISTA 4 mg prolonged-release tablets are pale beige and have "HM 4" printed in black ink on one side
- JURNISTA 8 mg prolonged-release tablets are red and have "HM 8" printed in black ink on one side
- JURNISTA 16 mg prolonged-release tablets are yellow and have "HM 16" printed in black ink on one side
- JURNISTA 32 mg prolonged-release tablets are white and have "HM 32" printed in black ink on one side
- JURNISTA 64 mg prolonged-release tablets are blue and have "HM 64" printed in black ink on one side.
JURNISTA is provided in blister packs of 14 tablets. Blister packs of 7, 10, 20, 28, 30, 35, 40, 50, 60 and 100 tablets are currently not marketed.
JURNISTA 4 mg (AUST R 155995)
JURNISTA 8 mg (AUST R 141508)
JURNISTA 16 mg (AUST R 141533)
JURNISTA 32 mg (AUST R 141534)
JURNISTA 64 mg (AUST R 141535)
Ingredients
Each JURNISTA tablet contains 4 mg, 8 mg, 16 mg, 32 mg or 64 mg of hydromorphone hydrochloride as the active ingredient.
Each tablet also contains the following other ingredients:
-
Coated tablet core:
polyethylene oxide, povidone, magnesium stearate, butylhydroxytoluene (E321), sodium chloride, hypromellose, iron oxide black (E172), lactose, cellulose acetate, macrogol 3350 and iron oxide yellow (E172) (32 mg tablet only). -
Colour overcoat:
lactose monohydrate, hypromellose, titanium dioxide (E171), glycerol triacetate, iron oxide red (E172) (4 mg & 8 mg tablet)/iron oxide black (4 mg tablet)/iron oxide yellow (E172) (4 mg & 16 mg tablet)/indigo carmine lake (E132) (64 mg tablet). -
Clear overcoat:
hypromellose and macrogol 400. -
Printing ink:
iron oxide black (E172), propylene glycol and hypromellose.
Sponsor
Janssen-Cilag Pty Ltd
1-5 Khartoum Road
Macquarie Park NSW 2113 Australia
Telephone: 1800 226 334
NZ Office: Auckland New Zealand
Telephone: 0800 800 806
This leaflet was prepared in October 2020.
OROS® formulation is a trademark of ALZA Corporation.
Published by MIMS December 2020

 No fixed conversion ratio is likely to be satisfactory in all patients, due to individual patient and formulation differences. Therefore, patients should be converted to the recommended starting dose of Jurnista followed by close monitoring and titration is advised.
No fixed conversion ratio is likely to be satisfactory in all patients, due to individual patient and formulation differences. Therefore, patients should be converted to the recommended starting dose of Jurnista followed by close monitoring and titration is advised.



 Steady-state plasma concentrations are approximately twice those observed following the first dose, and steady state is reached by the fourth dose of Jurnista. No time dependent change in pharmacokinetics was seen with multiple dosing. At steady state, Jurnista given once daily maintained hydromorphone plasma concentrations within the same concentration range as the immediate release tablet given 4 times daily at the same total daily dose and diminishes the periodic fluctuations in plasma levels seen with the immediate release tablet. The degree of fluctuation in plasma concentration at steady state during a 24 hour period (calculated as (Cmax(ss)- Cmin(ss))/Cavg(ss) x 100%) was lower with Jurnista (83%) as compared to the overall fluctuations of the immediate release tablet (147%) (see Figure 2). At steady state, hydromorphone AUC for Jurnista is equivalent to that observed for the immediate-release tablet.
Steady-state plasma concentrations are approximately twice those observed following the first dose, and steady state is reached by the fourth dose of Jurnista. No time dependent change in pharmacokinetics was seen with multiple dosing. At steady state, Jurnista given once daily maintained hydromorphone plasma concentrations within the same concentration range as the immediate release tablet given 4 times daily at the same total daily dose and diminishes the periodic fluctuations in plasma levels seen with the immediate release tablet. The degree of fluctuation in plasma concentration at steady state during a 24 hour period (calculated as (Cmax(ss)- Cmin(ss))/Cavg(ss) x 100%) was lower with Jurnista (83%) as compared to the overall fluctuations of the immediate release tablet (147%) (see Figure 2). At steady state, hydromorphone AUC for Jurnista is equivalent to that observed for the immediate-release tablet. Plasma protein binding is low (< 30%). Glucuronidation is the main metabolic pathway and the principal metabolite is the inactive hydromorphone 3-glucuronide, which follows a similar time course to hydromorphone in plasma. Unlike morphine, no active 6-glucuronide metabolite is produced. Linear pharmacokinetics has been demonstrated for the prolonged release tablet over the dose range 8 to 64 mg, with dose proportional increases in plasma concentrations (Cmax) and overall exposure (AUC).
Plasma protein binding is low (< 30%). Glucuronidation is the main metabolic pathway and the principal metabolite is the inactive hydromorphone 3-glucuronide, which follows a similar time course to hydromorphone in plasma. Unlike morphine, no active 6-glucuronide metabolite is produced. Linear pharmacokinetics has been demonstrated for the prolonged release tablet over the dose range 8 to 64 mg, with dose proportional increases in plasma concentrations (Cmax) and overall exposure (AUC). 4,5α-epoxy- 3-hydroxy-17- methyl-morphinan-6-one hydrochloride.
4,5α-epoxy- 3-hydroxy-17- methyl-morphinan-6-one hydrochloride.