What is in this leaflet
This leaflet answers some common questions about PANADOL EXTRA. It does not contain all the available information.
It does not take the place of talking to your pharmacist or doctor.
All medicines have risks and benefits.
If you have any concerns about using this medicine, ask your pharmacist or doctor.
Keep this leaflet with the medicine. You may need to read it again.
What PANADOL EXTRA is used for
The active ingredients in this medicine are paracetamol and caffeine. Paracetamol is used for the fast effective temporary relief of pain and discomfort associated with
- Headache
- Muscular aches
- Period pain
- Arthritis/Osteoarthritis
- Toothache
- Migraine headache
- Colds and flu
- Tension headache
- Sinus pain/headache
- Backache
Paracetamol also reduces fever.
Paracetamol works to stop the pain messages from getting through to the brain. It also acts in the brain to reduce fever.
Caffeine acts on paracetamol to increase its effectiveness.
Ask your pharmacist or doctor if you have any questions about this medicine. Your pharmacist or doctor may have given it for another reason.
Before you use PANADOL EXTRA
Do not take more than the recommended dose as it may cause serious harm to your liver.
When you must not use it
Do not use PANADOL EXTRA if you have an allergy to:
- Any of the ingredients listed at the end of this leaflet
Do not use this medicine if you are taking any other prescription or non-prescription medicines containing paracetamol to treat pain, fever, symptoms of cold and flu, or to aid sleep.
Always read and follow the label.
Do not use this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start using this medicine, talk to your pharmacist or doctor.
Before you start to use it
Tell your pharmacist or doctor if you have or have had any of the following medical conditions:
- Liver or kidney disease
- Are underweight or malnourished
- Regularly drink alcohol
You may need to avoid using this product altogether or limit the amount of paracetamol that you take. - You have a severe infection, are severely malnourished or are a chronic heavy alcohol user as this may increase the risk of metabolic acidosis.
Signs of metabolic acidosis include:
- deep, rapid, difficult breathing
- feeling sick (nausea), being sick (vomiting)
- loss of appetite
Contact a doctor immediately if you get a combination of these symptoms.
Please see your doctor if your symptoms do not improve.
Keep out of sight and reach of children.
Ask your pharmacist or doctor about using this medicine if you are pregnant or plan to become pregnant, or breastfeeding. Your pharmacist or doctor will discuss the benefits and possible risks of taking this medicine during pregnancy.
Consider taking the lowest effective dose for the shortest period of time.
If you have not told your pharmacist or doctor about any of the above, tell them before you use PANADOL EXTRA.
Using other medicines
Tell your pharmacist or doctor if you are using any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and paracetamol may interfere with each other. These include:
- Warfarin, a medicine used to prevent blood clots
- Metoclopramide, a medicine used to control nausea and vomiting
- Medicines used to treat epilepsy or fits
- Chloramphenicol, an antibiotic used to treat ear and eye infections
- Alcohol
- Probenecid, a medicine used to treat gout or sometimes given with an antibiotic
- Cholestyramine, a medicine used to treat high cholesterol levels in the blood
Your pharmacist and doctor will have more information on these and other medicines to be careful with or avoid while using this medicine.
How to use PANADOL EXTRA
Follow all directions given to you by your pharmacist or doctor carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your pharmacist or doctor for help.
Do not exceed the stated dose.
Use the smallest dose that you need to treat your symptoms and use the medicine for the shortest period of time necessary.
How much to use
Adults and children aged 12 years and over: Take 2 caplets every four to six hours as needed. Do not take more than 8 caplets in 24 hours.
Children under 12 years: Not recommended for children under 12 years of age.
Swallow with water or other fluid.
How long to use it
Adults:
Only take this medicine for a few days at a time unless your doctor tells you to take it for longer.
Children 12 to 17 years:
Only give this medicine to children for up to 48 hours unless a doctor has told you to give it for longer.
If you use too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26 for Australia, 0800 764 766 for New Zealand) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much PANADOL EXTRA. Do this even if there are no signs of discomfort or poisoning because of the risk of liver failure. You may need urgent medical attention.
While you are using PANADOL EXTRA
Things you must do
Talk to your pharmacist or doctor if your symptoms do not improve. Your pharmacist or doctor will assess your condition and decide if you should continue to take the medicine.
Things you must not do
Children 12 to 17 years:
Do not give this medicine for more than 48 hours unless a doctor has told you to.
Adults:
Do not use for more than a few days at a time unless your doctor tells you to.
Do not take more than the recommended dose unless your doctor tells you to.
Do not use PANADOL EXTRA to treat any other complaints unless your pharmacist or doctor tells you to.
Things to be careful of
Only drink small quantities of alcohol (beer, wine or spirits) while using paracetamol. Drinking large quantities of alcohol while taking paracetamol may increase the risk of liver side effects.
Side Effects
Tell your pharmacist or doctor as soon as possible if you do not feel well while you are using PANADOL EXTRA. This medicine helps most people with various types of pain but it may have unwanted side effects. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your pharmacist or doctor to answer any questions you may have.
If any of the following happen, tell your pharmacist or doctor immediately or go to Accident and Emergency at your nearest hospital:
- Shortness of breath
- Wheezing or difficulty breathing
- Swelling of the face, lips, tongue, throat or other parts of the body
- Rash, peeling, itching or hives on the skin or mouth ulcers
- Unexplained bruising or bleeding
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare for low doses of this medicine and when used for a short period of time.
If you have drinks or food containing caffeine while you are taking this medicine, you may experience caffeine-related side effects such as:
- Sleeplessness
- Restlessness
- Anxiety
- Irritability
- Headaches
- Stomach upsets
- Fast heartbeats
Tell your pharmacist or doctor if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
After using PANADOL EXTRA
Storage
Keep your medicine in the original pack until it is time to take it.
Keep your medicine in a cool dry place where the temperature stays below 25ºC.
Do not store PANADOL EXTRA or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in a car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
Ask your pharmacist what to do with any medicine that is left over, or if the expiry date has passed.
Product Description
What it looks like
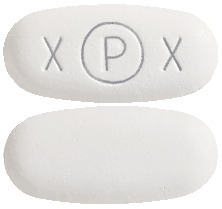
PANADOL EXTRA are white to off-white, film-coated tablets. On one side they are marked “xPx” with the “P” inside a circle. There are no markings on the other side. They come in blister packs of 10, 20 and 40 caplets.
Ingredients
PANADOL EXTRA contain 500 mg of paracetamol and 65 mg of caffeine as the active ingredients.
They also contain:
- Alginic acid
- Calcium carbonate
- Carnauba wax
- Crospovidone
- Magnesium stearate
- White colouring (Opadry YS-1R-7003)
- Povidone
- Sodium ethyl hydroxybenzoate
- Sodium methyl hydroxybenzoate
- Sodium propyl hydroxybenzoate
- Starch – pregelatinised maize
- Water - purified
Manufacturer/Supplier
PANADOL EXTRA is supplied in Australia and New Zealand by:
GlaxoSmithKline Consumer
Healthcare Australia Pty Ltd
82 Hughes Avenue, Ermington
NSW and Auckland, New Zealand
AUST R 203990
Date of preparation: August 2017
Trademarks are owned by or licensed to the GSK group of companies.
Published by MIMS November 2018



 When the recommended Panadol Extra dosing regimen is combined with dietary caffeine intake, the resulting higher dose of caffeine may increase the potential for caffeine related adverse effects such as insomnia, restlessness, anxiety, irritability, headaches, gastrointestinal disturbances and palpitations.
When the recommended Panadol Extra dosing regimen is combined with dietary caffeine intake, the resulting higher dose of caffeine may increase the potential for caffeine related adverse effects such as insomnia, restlessness, anxiety, irritability, headaches, gastrointestinal disturbances and palpitations.