1 Name of Medicine
Rifampicin.
2 Qualitative and Quantitative Composition
Rifadin 150 mg capsules contain 150 mg of rifampicin per capsule.
Rifadin 300 mg capsules contain 300 mg of rifampicin per capsule.
Rifadin syrup contains 100 mg of rifampicin per 5 mL of syrup.
Rifadin IV infusion contains 600 mg rifampicin per vial.
Excipients with known effect. Capsules. Contain sulfites.
Syrup. Contains methyl hydroxybenzoate, propyl hydroxybenzoate, potassium sorbate, sodium metabisulfite and saccharin.
For the full list of excipients, see Section 6.1 List of Excipients.
3 Pharmaceutical Form
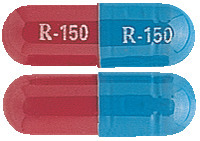
Capsules. 150 mg (blue/red, marked R-150).
300 mg (red, marked R-300).
Syrup. 100 mg/5 mL (red, raspberry flavoured).
IV infusion. 600 mg (spongy, fragile amorphous red powder) with 10 mL sterile water for injection solvent.
4 Clinical Particulars
4.9 Overdose
Symptoms. Nausea, vomiting, abdominal pain, pruritus, headache and increasing lethargy will probably occur within a short time after acute ingestion; actual unconsciousness may occur with severe hepatic involvement. Transient increases in liver enzymes and/or bilirubin may occur. Brownish-red or orange discolouration of the skin, urine, sweat, saliva, tears and faeces is proportional to amount ingested. Facial or periorbital oedema has also been reported in paediatric patients. Hypotension, sinus tachycardia, ventricular arrhythmias, seizures and cardiac arrest were reported in some fatal cases.
Liver enlargement, possibly with tenderness, can develop within a few hours after severe overdosage and jaundice may develop rapidly. Hepatic involvement may be more marked in patients with prior impairment of hepatic function. Other physical findings remain essentially normal. Direct and total bilirubin levels may increase rapidly with severe overdosage; hepatic enzyme levels may be affected, especially with prior impairment of hepatic function. A direct effect upon the haematopoietic system, electrolyte levels or acid base balance is unlikely.
Although it has not been observed in humans, animal studies suggest a possible neurodepressant action associated with very high doses of rifampicin. Where overdoses of other drugs, including such potentially hepatotoxic substances as isoniazid, pyrazinamide or ethionamide have occurred simultaneously, the signs and symptoms of acute poisoning may be aggravated and/or modified.
The minimum acute lethal or toxic dose is not well established. However, nonfatal acute overdoses in adults have been reported with doses ranging from 9 to 12 g of rifampicin. Fatal acute overdoses in adults have been reported with doses ranging from 14 to 60 g. Alcohol or a history of alcohol abuse was involved in some of the fatal and nonfatal reports. Nonfatal overdoses in paediatric patients aged 1 to 4 years old of 100 mg/kg for one to two doses have been reported.
Treatment. Intensive supportive and symptomatic measures should be instituted. Since nausea and vomiting are likely present, activated charcoal slurry instilled into the stomach following evacuation of gastric contents could help absorb any remaining drug in the gastrointestinal tract. Antiemetic medication may be required to control severe nausea/ vomiting.
Active diuresis (with measured intake and output) will help promote excretion of the drug. Bile drainage may be indicated in the presence of serious impairment of hepatic function lasting more than 24 to 48 hours; under these circumstances, extracorporeal haemodialysis may be required. In patients with previously adequate hepatic function, reversal of liver enlargement and impaired hepatic excretory function probably will be noted within 72 hours, with rapid return toward normal thereafter.
For information on the management of overdose, contact the Poisons Information Centre on 13 11 26 (Australia) or the National Poisons Centre on 0800 POISON.
5 Pharmacological Properties
5.3 Preclinical Safety Data
Genotoxicity. There are no known human data on the long-term potential for mutagenicity. There was no evidence of mutagenicity in bacteria, Drosophila melanogaster or mice. An increase in chromatid breaks was noted when whole-blood cell cultures were treated with rifampicin. Increased frequency of chromosomal aberrations was observed in vitro in lymphocytes obtained from patients treated with combinations of rifampicin, isoniazid and pyrazinamide, and combinations of streptomycin, rifampicin, isoniazid and pyrazinamide.
Carcinogenicity. There are no known human data on the long-term potential for carcinogenicity. A few cases of accelerated growth of lung carcinoma have been reported in man, but a causal relationship with the drug has not been established.
Rifampicin was associated with an increased incidence of liver tumours in the females of one strain of mice at doses from 2 to 10 times the recommended human therapeutic doses administered for 60 weeks. In another strain of mice and in rats, no increase of tumours was found. All these studies were carried out during most of the animals' life span.
Rifampicin has been reported to possess immunosuppressive potential in rabbits, mice, rats, guinea pigs, human lymphocytes in vitro and humans. Antitumor activity in vitro has also been shown with rifampicin.
6 Pharmaceutical Particulars
6.7 Physicochemical Properties
Rifampicin is a semisynthetic antibiotic derivative of rifamycin B. Specifically, rifampicin is the hydrazone, 3-(4-methylpiperazinyliminomethyl) rifamycin SV. It is only slightly soluble in water and is rather unstable to light and moisture.
Chemical structure.
https://stagingapi.mims.com/au/public/v2/images/fullchemgif/CSRIFAMP.gif C43H58N4O12.
CAS number. 13292-46-1.
7 Medicine Schedule (Poisons Standard)
S4 Prescription Only Medicine.
Summary Table of Changes
https://stagingapi.mims.com/au/public/v2/images/fulltablegif/RIFADIST.gif