SLINDA®
| Consumer Medicine Information (CMI) summary |
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
| 1. Why am I using Slinda? |
Slinda contains the active ingredient drospirenone. Slinda is a contraceptive pill and is used to prevent pregnancy.
For more information, see Section 1. Why am I using Slinda? in the full CMI.
| 2. What should I know before I use Slinda? |
Do not use if you have ever had an allergic reaction to Slinda or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I use Slinda? in the full CMI.
| 3. What if I am taking other medicines? |
Some medicines may interfere with Slinda and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
| 4. How do I take Slinda? |
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
Each blister of Slinda contains 24 white active tablets and 4 green placebo tablets. The two differently coloured tablets are arranged in order.
The first tablet of the treatment should be taken on the first day of menstrual bleeding. Thereafter, tablet taking is continuous.
More instructions can be found in Section 4. How do I take Slinda? in the full CMI.
| 5. What should I know while using Slinda? |
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using Slinda? in the full CMI.
| 6. Are there any side effects? |
Call your doctor straight away if you: have severe pain or swelling in either of your legs, unexplained chest pain, breathlessness, an unusual cough, if you cough up blood (possibly indicating a thrombosis); have a sudden, severe stomach ache or look jaundiced (possibly indicating liver problems); feel a lump in your breast (possibly indicating breast cancer); have a sudden or severe pain in the lower abdomen or stomach area (possibly indicating an ectopic pregnancy, this is a pregnancy outside the womb); are to be immobilised or are to have surgery (consult your doctor at least four weeks in advance); have unusual, heavy vaginal bleeding; suspect that you are pregnant.
Tell your doctor if you notice any of the following and they worry you: headache, tiredness, dizziness, mood changes, nausea, changes in weight, acne, sweating, breast tenderness or pain and changes in your period.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
SLINDA®
Active ingredient: Drospirenone
| Consumer Medicine Information (CMI) |
This leaflet provides important information about using Slinda. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using Slinda.
Where to find information in this leaflet:
1. Why am I using Slinda?
2. What should I know before I use Slinda?
3. What if I am taking other medicines?
4. How do I take Slinda?
5. What should I know while using Slinda?
6. Are there any side effects?
7. Product details
| 1. Why am I using Slinda? |
Slinda contains the active ingredient drospirenone. Slinda is a contraceptive pill and is used to prevent pregnancy. Each blister of Slinda contains 24 white tablets (also called active tablets) and 4 green tablets (also called placebo tablets) that do not contain active substance. The two differently coloured tablets are arranged in order.
Each of the 24 white active tablets contains a small amount of one type of female sex hormone, the progestogen drospirenone. For this reason Slinda is called a progestogen-only-pill (POP). POPs don't contain any estrogen hormone, so Slinda can be used by patients who do not tolerate estrogens.
Slinda provides high contraceptive efficacy. The contraceptive effect of Slinda is based on the inhibition of ovulation and changes in the cervical mucus, and effects on the endometrium, which becomes thinner.
Vaginal bleeding may occur at irregular intervals during the use of Slinda. You also may not have any bleeding at all.
| 2. What should I know before I use Slinda? |
Always check the ingredients to make sure you can use this medicine.
Do not use Slinda if:
- you are allergic to drospirenone, or any of the ingredients listed at the end of this leaflet.
- you have a blood clot in a blood vessel e.g. of the legs (deep venous thrombosis), or of the lungs (pulmonary embolism), or other organs.
- you have (or have ever had) liver disease and your liver function is still not normal.
- your kidneys are not working well (renal failure).
- you have or are suspected to have a cancer that is sensitive to sex-steroids, such as certain types of breast cancer.
- you have any unexplained vaginal bleeding.
If any of these conditions appear when using Slinda, stop taking this medicine and immediately contact your doctor.
Warnings
Check with your doctor if you:
- have ever had a thrombosis (formation of a blood clot in a blood vessel).
- have liver cancer, if you have jaundice (yellowing of the skin) or a liver disease and your liver is not working normally.
- have ever had a breast cancer.
- have or have had a chloasma (yellowish-brown pigmentation patches on the skin, particularly on the face); if this is the case, you will need to avoid exposure to the sun or ultraviolet radiation during treatment with Slinda.
- have diabetes.
- have high blood pressure.
- have kidneys that are not working well; your doctor will do a blood test to check your potassium levels during the first cycle.
- have any other medical conditions.
- take any medicines for any other condition.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
If you experience a worsening or first appearance of any of these conditions, you should contact your doctor.
Pregnancy and breastfeeding
Do not use Slinda if you are pregnant or think you might be pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Slinda may be used while you are breastfeeding.
No effects on breastfed newborns/infants are anticipated. However, very small amounts of drospirenone are excreted in breast milk.
Breast cancer
Regularly check your breasts and contact your doctor as soon as possible if you feel any lump in your breasts.
Breast cancer has been found slightly more often in patients who take other types of contraceptives that include a hormone called estrogen [these are called combined oral contraceptives (COCs) or combined Pills], than in patients of the same age who do not take the combined Pill. If patients stop taking the combined Pill, the risk gradually decreases, so that 10 years after stopping the risk is the same as for patients who have never taken the combined Pill.
Breast cancer is rare under 40 years of age. Breast cancers found in patients who take the combined Pill, seem less likely to spread than breast cancers found in patients who do not take the combined Pill. It is not known whether the difference in breast cancer risk is caused by the combined Pill. It may be that patients were examined more often, so that the breast cancer is noticed earlier.
The risk of breast cancer in users of progestogen-only pills like Slinda is believed to be similar to that in patients who use the combined Pill, but the evidence is less conclusive.
Thrombosis (formation of a blood clot in a blood vessel).
See your doctor immediately, if you notice possible signs of a thrombosis.
Thrombosis is the formation of a blood clot, which may block a blood vessel. A thrombosis sometimes occurs in the deep veins of the legs (deep venous thrombosis). If this clot breaks away from the veins where it is formed, it may reach and block the arteries of the lungs, causing a so-called “pulmonary embolism”.
There may be a slightly increased risk of thrombosis with progestogen-only pills. The risk of thrombosis is higher if a member of your family (a sibling or a parent) has had thrombosis at a relatively early age, with increasing age, obesity, prolonged immobilsation, major surgery or major trauma.
There is no apparent risk of having a heart attack or stroke (a blood clot in the brain) with a progestogen-only pill, unless you also have high blood pressure.
Bone metabolism
Treatment with Slinda leads to decreased hormone (estradiol) levels, to a level corresponding with the early phase of the menstrual cycle. It is currently unknown whether the decrease in this hormone level may have a clinically relevant effect on bone mineral density. Loss of bone mineral density is of particular concern during adolescence and early adulthood, a critical period of bone accretion. It is unknown if bone mineral density decrease in this population will reduce peak bone mass and increase the risk for fracture in later life. Your doctor will decide if Slinda is an appropriate treatment for you, taking into account if you have significant risk factors for osteoporosis.
Psychiatric disorders
Some patients using hormonal contraceptives including Slinda have reported depression or depressed mood. Depression can be serious and may sometimes lead to suicidal thoughts. If you experience mood changes and depressive symptoms contact your doctor for further medical advice as soon as possible.
Medical examination
Before you start taking Slinda for the first time or if you re-start the treatment after some time of not taking it, your doctor will ask you some questions about your health and will do a complete physical examination, including blood pressure measurements. Your doctor will tell you how often you should go for control visits.
Children and adolescents
Slinda is used after menarche (the first menstrual bleeding).
| 3. What if I am taking other medicines? |
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with Slinda and affect how it works. These include medicines used for the treatment of:
- epilepsy (e.g. primidone, phenytoin, barbiturates, carbamazepine, oxcarbazepine, felbamate, topiramate)
- tuberculosis (e.g. Rifampicin, rifabutin)
- HIV infections (e.g. ritonavir, nevirapine, nelfinavir) or other infectious diseases (e.g. griseofulvin)
- Hepatitis C Virus infections (e.g. boceprevir, telaprevir)
- high blood pressure in the blood vessels in the lungs (e.g. bosentan)
- depressive mood (e.g. herbal remedy St. John's wort)
- certain bacterial infections (e.g. clarithromycin, erythromycin)
- fungal infections (e.g. fluconazole, itraconazole, ketoconazole, voriconazole)
- high blood pressure (hypertension), angina or certain heart rhythm disorders (e.g. diltiazem)
Your doctor can tell you if you need to take additional contraceptive precautions (for example condoms) and if so, for how long.
Slinda may also influence the effect of other medicines, causing either an increase in effect (e.g. cyclosporine) or a decrease in effect (e.g. lamotrigine).
If Slinda is taken at the same time as potassium-sparing diuretics or aldosterone antagonists, which can increase serum potassium levels, your doctor could recommend testing your serum potassium levels during the first treatment cycle with Slinda.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect Slinda.
Avoid grapefruit or grapefruit juice while you are taking Slinda.
| 4. How do I take Slinda? |
How much to take
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
Each blister of Slinda contains 24 white active tablets and 4 green placebo tablets.
Take one tablet of Slinda every day with a little water if necessary. You may take the tablets with or without food. You must take the tablets every day around the same time of the day so the interval between two tablets is always 24 hours.
Do not confuse the tablets:
- Because of the different composition of the tablets it is necessary to begin with the first white active tablet on the upper left and to take the tablets every day.
- For the correct order, follow the direction of the arrows and the sequence of numbers on the blister.
- The first tablet of the treatment should be taken on the first day of menstrual bleeding. Thereafter tablet taking is continuous.
- Take a white active tablet for the first 24 days and then a green placebo tablet for the last 4 days.
- You must then start a new pack straightaway (24 white active tablets followed by 4 green placebo tablets) without a break in daily tablet intake. There is therefore no gap between two packs.
You may have some bleeding during the use of Slinda, or you may also have no bleeding at all, but you must continue to take your tablets as normal without interruption.
If you use Slinda in this manner, you are still protected against pregnancy during the 4 days when you are taking a placebo tablet.
If you start taking the first pack of tablets on days 2 to 5 of the menstrual cycle a barrier method should be used until you have completed 7 days of uninterrupted white active tablets.
Preparation of the blister
To help you keep track, stickers, each with the 7 days of the week are provided in the pack.
Choose the sticker that starts with the day you begin taking the tablets (for example, if you start menstruating on a Thursday, use the sticker that starts with “THU”) and place it on the blister card over the words “Place day label here” so that the first day is above the tablet marked “START”.
There will be a day indicated above every tablet, so you can see whether you have taken a certain pill. The arrows and the consecutive numbers show the order you are to take the pills.
Starting your first pack of Slinda
If you have not used a hormonal contraceptive in the previous month
Begin with Slinda on the first day of your period. When doing so, you are immediately protected against pregnancy and you do not need to use extra protective measures such as a condom.
If you start Slinda on days 2 to 5 of your period you must use extra protective measures such as a condom until you have taken 7 white active tablets.
When changing from a combined pill, vaginal ring or transdermal patch
Option 1
You should start Slinda on the day:
- after the last active tablet (the last tablet containing the active substances) of your previous pill or
- on the day of removal of your vaginal ring or
- on the day of removal of your transdermal patch
This means no tablet, ring or patch-free break.
If you follow these instructions, no additional contraceptive precautions are necessary.
Option 2
You can also start Slinda, at the latest, on the day following either:
- the placebo interval of your present contraceptive tablet or
- the hormone-free interval following removal of your vaginal ring or
- a patch-free break
In these cases, make sure you use an additional barrier method of contraception for the first 7 days of taking Slinda.
When changing from another progestogen-only pill (POP)
You may switch any day from another POP and start taking Slinda the next day. Additional contraceptive precautions are not necessary.
When changing from a progestogen-only-injection or implant or from a progestogen-releasing intrauterine system (IUS)
You should start Slinda the day when the next injection is due or on the day that your implant or your IUS is removed. Additional contraceptive precautions are not necessary.
After having a baby
You can start Slinda any day between day 21 to 28 after having your baby. If you start later than day 28, but before the menstruation has returned, you must be sure you are not pregnant and you must use a barrier method such as a condom until you have completed the first 7 days of tablet-taking.
After miscarriage
You should follow the advice of your doctor.
When to take Slinda
- Take one tablet of Slinda every day at about the same time of the day so that the interval between two tablets is always 24 hours.
If you forget to take Slinda
Slinda should be used regularly at the same time each day. If you are less than 24 hours late in taking any active white tablet, contraceptive protection is not reduced. You should take the tablet as soon as you remember and take further tablets at the usual time without further contraceptive protection being required.
If you are more than 24 hours late in taking any white active tablet, contraceptive protection may be reduced. Refer to the table below for further instructions. The more consecutive tablets you have missed, the higher the risk that the contraceptive efficacy is decreased.
Instructions for missed Slinda tablets
| Days during cycle | Instructions for missed tablet if you are more than 24 hours late |
| Days 1 – 7 | Take the missed tablet as soon as you remember even if this means taking two tablets at the same time and use an additional method of contraception for the next 7 days. |
| Days 8 – 17 | Take the missed tablet as soon as you remember, even if that means taking two tablets at the same time. Continue taking the white active tablets at the usual time. If you have taken the active white tablets correctly in the 7 days before the first missed tablet, no additional contraceptive protection is required. If you have missed more than one tablet, then extra contraceptive precautions should be used until you have taken 7 days of uninterrupted white active tablets. |
| Days 18 – 24 | Two options are possible in this time frame as follows:
|
The last 4 green tablets in the 4th row of the strip are the placebo tablets. If you forget one of these tablets, this has no effect on the reliability of Slinda. Throw away the forgotten placebo tablet.
If you have missed tablets and you do not experience a withdrawal bleed in the placebo tablet interval, the possibility of pregnancy should be considered.
What to do in the case of vomiting or severe diarrhoea
If you vomit or have severe diarrhoea, there is a risk that the active substance in the pill will not be fully absorbed by your body, the situation is almost the same as forgetting a tablet. In these cases, an additional method of contraception may be needed, ask your doctor for advice.
If you vomit or have severe diarrhoea within 3-4 hours after taking your white active tablet of Slinda, you must take another white tablet from another blister pack as soon as possible. If possible, take it within 12 hours of when you normally take your pill. Additional contraceptive precautions are not necessary. If this is not possible or 12 hours have passed, you should follow the advice given in the section “If you forget to take Slinda” above.
If you use too much Slinda
There have been no reports of serious harmful effects from taking too many Slinda tablets at one time.
Symptoms that may occur are nausea, vomiting and slight vaginal bleeding.
If you think that you have used too much Slinda you should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
However, in case of overdose, ask your doctor for advice because blood tests should be done.
| 5. What should I know while using Slinda? |
Slinda contains lactose (milk sugar). If you have an intolerance to some sugars, contact your doctor before you start to take Slinda.
Things you should do
Regular check-ups
When you are using Slinda, your doctor will tell you to return for regular check-ups. In general, the frequency and nature of these check-ups will depend on your personal situation.
Call your doctor as soon as possible if you:
- have severe pain or swelling in either of your legs, unexplained pains in the chest; breathlessness, an unusual cough, especially when you cough up blood (possibly indicating a thrombosis);
- have a sudden, severe stomach ache or look jaundiced (possibly indicating liver problems);
- feel a lump in your breast (possibly indicating breast cancer);
- have a sudden or severe pain in the lower abdomen or stomach area (possibly indicating an ectopic pregnancy, this is a pregnancy outside the womb);
- are to be immobilised or are to have surgery (consult your doctor at least four weeks in advance);
- have unusual, heavy vaginal bleeding;
- suspect that you are pregnant.
Remind any doctor, dentist or pharmacist you visit that you are using Slinda.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Slinda affects you.
No effects on ability to drive and use machines have been observed in users of oral hormone contraceptives, although no studies have been performed with Slinda.
Looking after your medicine
Keep this medicine out of the sight and reach of children.
Store below 25°C.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date which is stated on the packaging after EXP. The expiry date refers to the last day of that month.
| 6. Are there any side effects? |
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
Changes in your reproductive system
| Speak to your doctor if you have any of these less serious side effects and they worry you |
Serious side effects
| Serious side effects | What to do |
Other side effects such as:
refer to Section 5 ‘What should I know while using Slinda?’ for additional precautions. | Call your doctor straight away, or go to the Emergency Department at the nearest hospital if you notice any of these serious side effects or worsening of conditions that you may already have. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
| 7. Product details |
This medicine is only available with a doctor's prescription.
What Slinda contains
| Active ingredient (main ingredient) | Drospirenone 4 mg |
| Other ingredients (inactive ingredients) | White active film coated tablets: Microcrystalline cellulose Lactose Colloidal anhydrous silica Magnesium stearate Polyvinyl alcohol Titanium dioxide Macrogol 3350 Purified-Talc Green placebo film coated tablets: Lactose monohydrate Maize Starch Povidone Colloidal anhydrous silica Magnesium stearate Hypromellose Triacetin Polysorbate 80 Titanium dioxide Indigo carmine Iron oxide yellow |
| Potential allergens | Lactose |
Do not take this medicine if you are allergic to any of these ingredients.
What Slinda looks like
Each blister of Slinda contains 24 white active film-coated tablets and 4 green placebo film-coated tablets.
The active tablet is a round, white tablet with the letters “E” and “D” debossed on opposite sides, with a diameter of 5 mm.
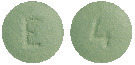
The placebo tablet is a round, green tablet with the letter “E” and the number “4” debossed on opposite sides, with a diameter of 5 mm.
AUST R 338904
Who distributes Slinda
Besins Healthcare Australia Pty Ltd
Level 16, Tower 2, Darling Park,
201 Sussex Street, Sydney NSW 2000
This leaflet was prepared in June 2021.

By scanning the QR code with your smart phone or tablet, you can access patient information on Slinda®.
Access only available within Australia.
Published by MIMS August 2021