Dr Jill Thistlethwaite, NPS MedicineWise medical adviser and a Sydney GP, understands that helping patients to lose weight is hard.

‘There are no simple solutions. It takes time and effort, and can feel frustrating when any changes in weight are slow to occur, which is not uncommon’, she says.
How uncommon was investigated in a recent study of the probability of weight loss in over 176,000 primary care patients in the UK with a Body Mass Index (BMI) of 30.0–34.9 kg/m2. During a maximum 9-year follow up, it found the annual probability of a 5% weight reduction was 1 in 10 for women; 1 in 12 for men. As expected, the annual odds of reaching a normal weight (defined as BMI 18.5 to 24.9 kg/m2) were even worse: 1 in 124 for women; 1 in 210 for men.1
There is a lack of evidence in the literature for lifestyle intervention achieving significant, sustained weight loss in primary care.2,3 But despite potentially discouraging outcomes, GPs like Dr Thistlethwaite persevere, and continue to play an important role helping patients manage their weight.4
Dr Thistlethwaite’s approach includes not allowing frustration to prevent her from seeing opportunities to get better at facilitating weight loss.
As a result, Dr Thistlethwaite has improved her approach to her patients’ weight management over time. ‘When I was a less experienced GP, it was all black and white. I would just tell patients what they needed to do and expect they’d get it done’, she says.
‘However, as I got more experienced, I learnt to see people as individuals. It was in the mid-1990s that it became clear for me that as with medication adherence, just telling a patient what to do is rarely successful in the longer term.’
This approach has enabled Dr Thistlethwaite to identify that osteoarthritis is an opportunity for her to discuss and monitor weight loss with her patients over time.
‘The development of early stage osteoarthritis can be a trigger to help patients with the motivation required to lose weight. It can also help them be more agreeable to exercise if you provide an updated understanding of osteoarthritis that it’s not a ‘wear and tear’ disease and that exercise will not cause damage to the joint’, says Dr Thistlethwaite.
‘For patients with advanced osteoarthritis who are waiting for joint replacement surgery, it’s not too late to stress how beneficial weight loss is,” she says.
‘These are opportunities for better weight management that GPs might find beneficial in their clinical practice.’
Download and print
Weight loss is core osteoarthritis treatment
Being overweight or obese is the single most important risk factor for knee osteoarthritis (OA).5 People who are obese are twice as likely to develop knee OA compared to non-obese people; the lifetime risk is 20% compared to 11%.6
And weight loss stands tall among OA management options. Whereas oral analgesics only have an adjunctive role (such as to enable exercise and maintain physical function),7 international guidelines recommend weight loss as a core treatment.8-10
A 2007 meta-analysis of 4 randomised controlled trials found a weight reduction of 6.1 kg (95% CI, 4.7 to 7.6 kg) reduced self-reported pain and disability with pooled effect sizes of 0.20 (95% CI, 0 to 0.39) and 0.23 (95% CI, 0.04 to 0.42) respectively.11 These effect sizes were small, but clinically significant and comparable to the modest effect sizes from non-steroidal anti-inflammatory drugs (without the risk of drug-related harms).5,12 A subsequent 2013 randomised controlled trial (RCT) that found similar results has added strength to these findings.13
All these studies were conducted on knee OA, however, which makes it difficult to generalise the results to the hip. While the link between obesity and hip OA is less well established, guidelines are clear that weight loss is recommended for OA in general due to the associated general health benefits, particularly for patients with concurrent chronic diseases.7,9,14
It’s this overlap of management of OA and other chronic diseases that Dr Thistlethwaite has found provides an opportunity for helping patients get started with weight loss.
Osteoarthritis can be a better motivator
The recommendation to lose weight is not the only thing chronic diseases such as OA, cardiovascular disease (CVD) and type 2 diabetes have in common.7,8,10,14 Most patients with OA have at least one concurrent condition; in fact 51% have CVD, and 14% have type 2 diabetes.7,15 See Figure 1 below.
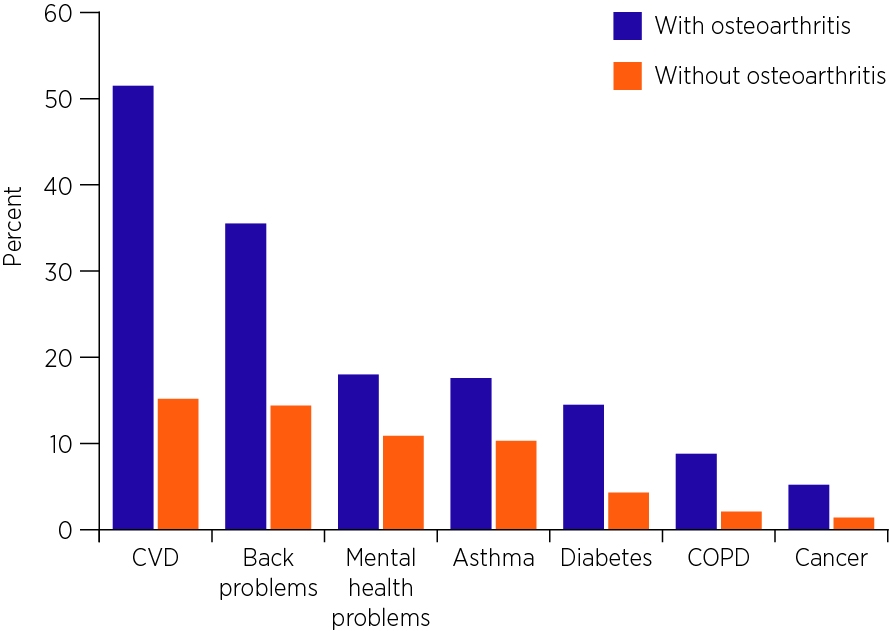
Figure 1: Prevalence of other chronic conditions in people with OA compared to people without OA, 2014–15
Dr Thistlethwaite says OA can be a better motivator for weight loss than other chronic diseases.
‘For instance, the problem with type 2 diabetes – if the patient doesn’t have symptoms – is that the benefits of secondary prevention are all in the future. That may make them seem less real and, as a result, more difficult to explain and less motivating for implementing lifestyle change’, she says.
‘But with osteoarthritis, you can connect symptoms to something immediate that patients can understand or benefits they can experience within a short period of time. As a result, you may be more successful achieving weight loss by focussing on their OA symptoms.’
Associate Professor Ilana Ackerman from Monash University’s Department of Epidemiology and Preventive Medicine, who is an experienced physiotherapist, says that a diagnosis of OA can offer an opportunity for helping patients with their weight management, which she regards as a ‘teachable moment’ for health behaviour change.

Associate Professor Ilana Ackerman: Reducing pain can be a great motivator.
‘If you tell me I can have treatment that will give me tangible benefits in one month or another treatment that will help in 10 years, I’m going to be more inclined towards the short-term benefit’, says Associate Professor Ackerman.
‘We know in clinical practice that reduction in pain can be a great motivator for patients. So can improved function, such as explaining to a patient that functional improvements after weight loss can enable them to walk down to the shops or fulfil important family roles like caring for their grandchildren’, she says.
Qualitative research has highlighted some key motivations among people with OA with regard to weight loss. A 2017 study involved interviews with patients with knee OA, pre and post-joint replacement surgery, who had successfully lost weight. They reported that, along with physical appearance, how their clothing fitted and preventing knee replacement surgery, improving symptoms was a key motivation.16
Ensuring a correct understanding of osteoarthritis
Helping patients understand their OA through education is another opportunity for facilitating better management of weight loss, says Dr Thistlethwaite.
Patient education is best described as an information-sharing process.9 ‘You share information with the patient about osteoarthritis and the patient informs you about themselves such as their knowledge, needs and preferences’, says Dr Thistlethwaite.
Information should be provided to the patient on the current understanding of OA as a multi-factorial disease affecting the whole joint – cartilage, bone, synovium, muscles and ligaments7,9,17 – in a way that is tailored to their health literacy and individual needs.
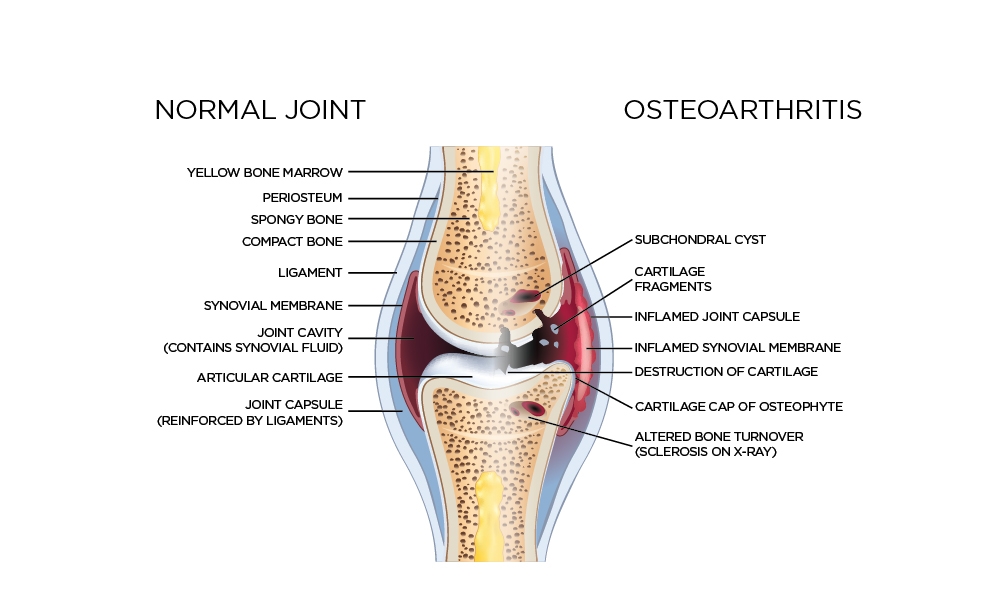
Figure 2: OA is a multi-factorial disease affecting the whole joint, not just the articular cartilage.18
These factors include not only genetics, gender and age, but also modifiable factors such as injury, joint malalignment and excess weight – and they all contribute to produce joint failure, via mechanical and systemic pathways.7,17
‘It’s still very common for patients to believe that OA is simply a degenerative “wear and tear” disease of the cartilage that’s an inevitable part of ageing’, says Associate Professor Ackerman.
‘In part this is because this is what we as clinicians have told our patients for many years, but as new evidence comes to light we need to re-think how we explain OA to our patients, and we also need to re-think the terms we use to describe the condition, such as "bone on bone"’, she says.
Adding to the misunderstanding are reputable websites in Australia and overseas that still haven’t updated their content to reflect current thinking.
The concern is that when patients think of OA as a ‘wear and tear’ disease, it can act as a deterrent for doing exercise and remaining physically active.
‘Patients often believe that exercise will wear out the joint quicker. Many also have pain during physical activity, so doing exercise as a treatment can be counter-intuitive’, says Dr Thistlethwaite.
‘You can explore the patient’s understanding by asking “What do you think OA is?” and if they have a misunderstanding, providing accurate information about the condition and about what they can expect to feel during and after exercise can help motivate them to participate in regular exercise’, she says.
Fat and lipids
At the same time that Dr Thistlethwaite was learning to consult with her patients in new ways in the mid-1990s, OA and obesity researchers began shedding new light on the pathology of OA.19,20
They found that obesity was an increased risk factor for OA of the hand joints.17 Clearly, as the hand is not a weight-bearing structure, scientists realised that more than just the traditional mechanical pathway was involved. So they began looking for evidence of a systemic pathway.
The focus settled on body fat.21 Rather than being an inert substance that keeps you warm or makes your clothes feel tighter, there was evidence that it’s also an active tissue that secretes biochemicals, particularly adipokines and cytokines such as interleukin 6 (IL-6), which generate low-grade inflammation.22
Dyslipidaemia was found to be another systemic pathway contributor to OA. Lipids such as triglycerides have pro-inflammatory properties and abnormally high levels may further aggravate systemic inflammation.22
Clinical research supports the above pathology findings. An Australian prospective cohort study found for knee and hip OA that not only BMI, but also fat mass was associated with a 3–4-fold risk of joint replacement surgery (when comparing fourth and first quartile).23
Figure 3: Systemic and mechanical pathways leading to OA22
Reproduced with permission
A Danish RCT of weight loss for knee OA found that every 1% reduction in body fat was more than 3 times more powerfully associated with improvements in pain, function and stiffness compared to every 1% body weight reduction (9.4% versus 2.8% improvement).24
In fact, interest in dyslipidaemia and OA has prompted researchers to investigate if statins can offer benefits for OA. Cohort studies have already found that statins are associated with a reduced incidence and progression of OA.25,26 An Australian RCT is now looking at whether statins can actually reverse the progression of knee OA.27 Results are expected in early 2018.28
For all the interest in a systemic pathway, however, the mechanical pathway leading to OA shouldn’t be forgotten. It is seen clearly in patients who lose weight.
Dr Thistlethwaite says ‘You can explain the impact to the patient. You can ask: “Does carrying heavy shopping make your joints more painful?” You can then say: “Then imagine the pain reduction of carrying around less weight on your body.”’
Explaining the systemic pathway behind OA may also help patients who want this level of detail by indicating that losing weight can decrease inflammation by reducing fat and improving lipids, she says.
Let's talk about weight
It’s not just patients who might need help. GPs and other health professionals may also need help with raising the sensitive issue of weight with patients due to insufficient confidence to manage weight loss and feeling a lack of efficacy following repeated failed efforts and outcomes.3,4
‘A useful approach is to include weight as part of a more general discussion about the patient’s health and individualised management plan’, says Associate Professor Ackerman.

‘You can let the patient know, for instance, that current guidelines consistently recommend that the core treatments for OA include patient education, self-management and exercise, as well as weight loss’, she says.
‘You can then ask the patient about their thoughts on weight loss, including previous attempts and strategies they may have used, and take the discussion from there.’
What is the recommended weight loss goal for patients with OA to reduce pain and improve function?
There is evidence that improvement in symptoms and function is proportional to the percentage of weight loss.7,31 So clearly, the more weight loss, the better. As a result, some studies and experts are suggesting that ≥ 10% of body weight should be the recommended goal.13,30,32 Current Australian guidelines are more modest, however, stating that a reasonable target is > 5% weight reduction.7,8
Diet and exercise advice
Once a patient is motivated to lose weight, the first-line management is usually diet and exercise. But which one is better?
The answer is they’re better together. A 2013 RCT of 339 patients with knee OA found that while the amount of weight loss achieved by exercise alone was 2 kg, and for diet alone 9 kg, diet and exercise combined achieved a loss of nearly 11 kg.13
Fortunately, the recommendations for what to eat and drink, and what exercise to do, are closely aligned between OA-specific and general weight loss guidelines. They include the following advice.
Diet
The 2013 European League Against Rheumatism (EULAR) guidelines generally recommend:
- healthy eating
- reducing fat and sugar
- limiting salt intake
- eating at least five portions of fruit and vegetables a day
- self-monitoring
- explicit weight-loss goals, and
- motivational interviewing.33
Exercise
The physical activity recommendation for weight loss – taking into account both OA-specific and general obesity guidelines – is 150 to 300 minutes of moderate intensity aerobic exercise each week.14,33-35 The 2013 EULAR guidelines provide more specific advice on what exercises to do and how to do them.
For older people who can’t do this amount because of chronic conditions, they should be as physically active as their abilities allow.35
It may also be helpful to consider exercise as part of a holistic approach to managing patients with multimorbidity, including OA, which prioritises which condition to treat first.36
Appropriate exercise can be undertaken safely in a variety of settings such as the home, gym, group class or under clinical supervision.7
Associate Professor Ackerman says if weight-bearing exercise is not possible due to pain, water-based exercise may be appropriate, depending on co-existing medical conditions. When considering an appropriate exercise program for OA, advice should be sought from a suitably qualified health professional, such as a physiotherapist, who can tailor a targeted exercise program to the individual’s requirements and modify and progress the program as needed.
Australian OA guidelines recognise, however, that patients often need additional encouragement to undertake exercise because of joint pain and perceived instability.7
‘Reassure patients that some discomfort at the affected joint during and/or after exercise is likely and this does not indicate disease progression’, they advise.7
‘Encourage patients using supportive and non-catastrophic language such as ‘hurt does not mean harm’ and ‘sore but safe’. Topical or oral analgesia may be required to facilitate exercise.'7
Dr Thistlethwaite has found these principles can be explored with the patient to develop a prescription for exercise that takes into account what they might like to do. It’s all part of seeing the patient as an individual and understanding their needs and motivations to help make their weight management more effective, she says.
Expert reviewer
Associate Professor Ilana Ackerman
Department of Epidemiology and Preventive Medicine
Monash University
References
- Fildes A, Charlton J, Rudisill C, et al. Probability of an obese person attaining normal body weight: Cohort study using electronic health records. Am J Public Health 2015;105:e54-9.
- Booth HP, Prevost TA, Wright AJ, et al. Effectiveness of behavioural weight loss interventions delivered in a primary care setting: a systematic review and meta-analysis. Fam Pract 2014;31:643-53.
- Ashman F, Sturgiss E, Haesler E. Exploring self-efficacy in Australian general practitioners managing patient obesity: A qualitative survey study. Int J Family Med 2016;2016:8212837.
- Harris MF, Spooner CJ. Weight loss options in general practice. Med J Aust 2014;201:184-5.
- Yu SP, Hunter DJ. Managing osteoarthritis. Aust Prescr 2015;38:115-9.
- Losina E, Weinstein AM, Reichmann WM, et al. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken) 2013;65:703-11.
- Rheumatology Expert Group. Therapeutic Guidelines: Osteoarthritis. West Melbourne, Victoria: Therapeutic Guidelines Ltd, 2017 (accessed 30 November 2020).
- Australian Commission on Safety and Quality in Health Care. Osteoarthritis of the Knee Clinical Care Standard. Sydney: ACSQHC, 2017 (accessed 30 November 2020).
- National Institute for Health and Care Excellence. Osteoarthritis, Care and management in adults. London: National Clinical Guideline Centre (UK), 2014 (accessed 30 November 2020).
- McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22:363-88.
- Christensen R, Bartels EM, Astrup A, et al. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 2007;66:433-9.
- Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage 2010;18:476-99.
- Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA 2013;310:1263-73.
- National Health and Medical Research Council. Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. Melbourne: NHMRC, 2013 (accessed 30 November 2020).
- Australian Institute of Health and Welfare. Osteoarthritis. Canberra: AIHW, 2020 (accessed 30 November 2020)
- Pellegrini CA, Ledford G, Hoffman SA, et al. Preferences and motivation for weight loss among knee replacement patients: implications for a patient-centered weight loss intervention. BMC Musculoskelet Disord 2017;18:327
- Martel-Pelletier J, Barr AJ, Cicuttini FM, et al. Osteoarthritis. Nat Rev Dis Primers 2016;2:16072.
- Robinson WH, Lepus CM, Wang Q, et al. Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat Rev Rheumatol 2016;12:580-92.
- Gomez R, Lago F, Gomez-Reino J, et al. Adipokines in the skeleton: influence on cartilage function and joint degenerative diseases. J Mol Endocrinol 2009;43:11-8.
- Conway R, McCarthy G. Obesity and osteoarthritis: more than just mechanics. EMJ Rheumatology. 2015; 2: 75-83 (accessed 30 November 2020).).
- Cicuttini FM, Wluka AE. Not just loading and age: the dynamics of osteoarthritis, obesity and inflammation. Med J Aust 2016;204:47
- Thijssen E, van Caam A, van der Kraan PM. Obesity and osteoarthritis, more than just wear and tear: pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity-induced osteoarthritis. Rheumatology (Oxford) 2015;54:588-600
- Wang Y, Simpson JA, Wluka AE, et al. Relationship between body adiposity measures and risk of primary knee and hip replacement for osteoarthritis: a prospective cohort study. Arthritis Res Ther 2009;11:R31.
- Christensen R, Astrup A, Bliddal H. Weight loss: the treatment of choice for knee osteoarthritis? A randomized trial. Osteoarthritis Cartilage 2005;13:20-7.
- Kadam UT, Blagojevic M, Belcher J. Statin use and clinical osteoarthritis in the general population: a longitudinal study. J Gen Intern Med 2013;28:943-9.
- Clockaerts S, Van Osch GJ, Bastiaansen-Jenniskens YM, et al. Statin use is associated with reduced incidence and progression of knee osteoarthritis in the Rotterdam study. Ann Rheum Dis 2012;71:642-7
- Wang Y, Tonkin A, Jones G, et al. Does statin use have a disease modifying effect in symptomatic knee osteoarthritis? Study protocol for a randomised controlled trial. Trials 2015;16:584.
- Jones G. OAKS trial. Personal Communication. 21 August 2017.
- Messier SP, Gutekunst DJ, Davis C, et al. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum 2005;52:2026-32.
- Aaboe J, Bliddal H, Messier SP, et al. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthritis Cartilage 2011;19:822-8
- Atukorala I, Makovey J, Lawler L, et al. Is there a dose-response relationship between weight loss and symptom improvement in persons with knee osteoarthritis? Arthritis Care Res (Hoboken) 2016;68:1106-14
- Garett N. Everyday arthritis treatments: what works? ABC Health & Wellbeing. Sydney: ABC, 2014 (accessed 30 November 2020).
- Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013;72:1125-35.
- Cardiovascular Expert Group. Therapeutic Guidelines. Physical activity and cardiovascular disease risk. West Melbourne, Victoria: Therapeutic Guidelines Ltd, 2018 (accessed 17 December 2021).
- Bennell KL, Hinman RS. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport 2011;14:4-9.
- Harris MF, Dennis S, Pillay M. Multimorbidity: negotiating priorities and making progress. Aust Fam Physician 2013;42:850-4.
